As one of the most prominent endometriosis specialists in the world, Dr. Farr Nezhat is known for managing severe, multi-organ endometriosis. His pioneering utilization of minimally invasive laparoscopic and robotic procedures to safely treat endometriosis and gynecological cancers has cemented his practice as a leading global option for recognizing, treating, and preventing cancers that arise from endometriosis.
How should we approach treatment of women with endometriosis to detect and prevent ovarian cancer?
Once women with endometriosis are identified, either surgically documented or by self‐reported symptoms, they should be managed as follows:
- Hormonal treatment or, if already desired, possible pregnancy, aimed at reducing the risk of recurrent endometriosis and endometriomas
- Careful follow up of presumed ovarian endometriomas with imaging studies, particularly MRI when ultrasound is suspicious, to detect any characteristic changes such as mural formation or rapid enlargement, which may be suspicious for cancer
- Complete surgical resection when possible of all endometriotic foci in women undergoing surgical treatment, with tissue evaluation to rule out malignancy
- Oophorectomy and salpingectomy should be individualized and offered based on the patient’s age, familial risk of ovarian cancer, ovarian and fallopian tube damage, etc.
- Fertility preservation – embryo, egg or ovarian tissue preservation should be considered
What is the risk of malignant transformation of endometriosis?
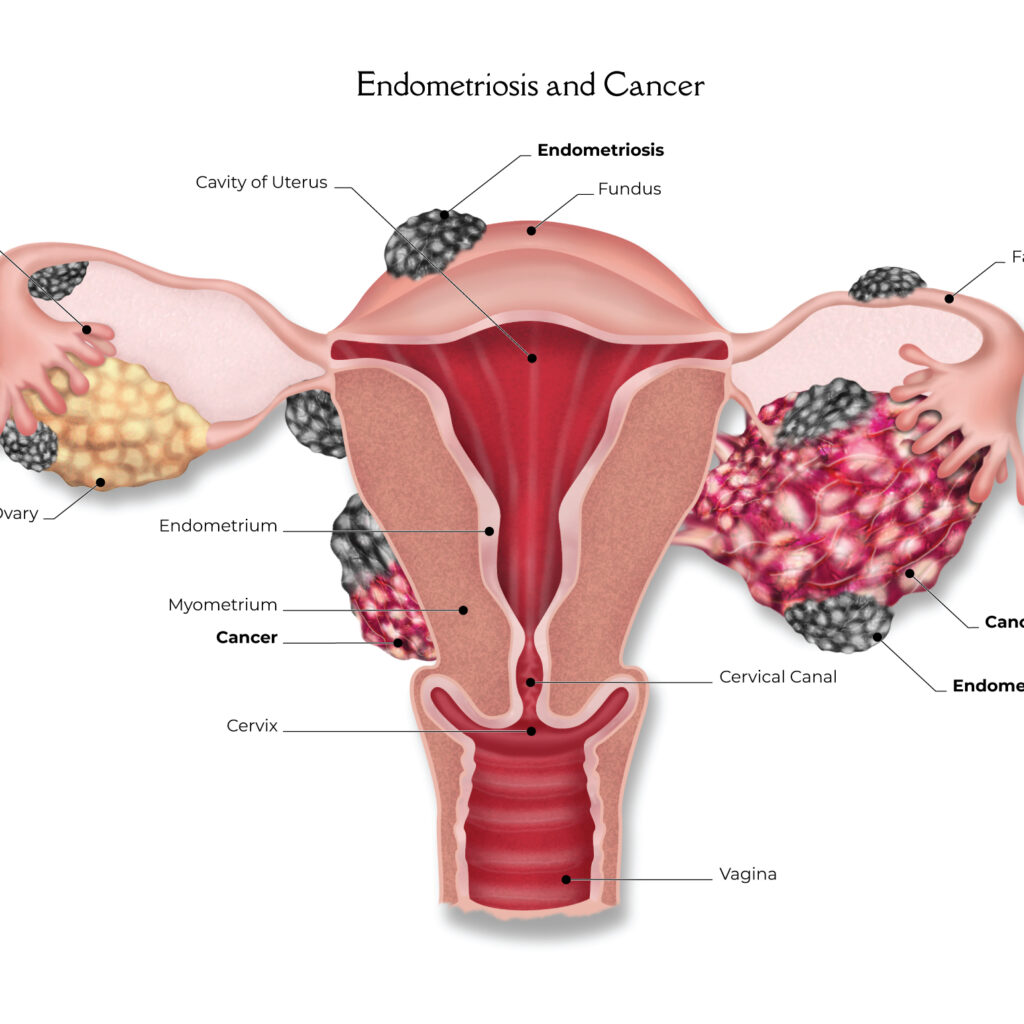
The transformation of ovarian and non-ovarian endometriosis to certain histological type malignancies is well established and has perplexed physicians for a long time. Sampson first suggested the malignant transformation of endometriosis in 1925 (1,2,3,6). Epidemiological studies have suggested a link between endometriosis and ovarian low-grade serous, endometrioid, clear-cell ovarian, and extra-ovarian cancers.
In a study reported in Lancet Oncology, a team of researchers from the Ovarian Cancer Association Consortium (OCAC) performed a pooled analysis of 13 case-control studies and confirmed that women with self-reported history of endometriosis have a significantly increased risk of clear cell carcinoma (odds ratio 3.05) and endometrioid ovarian cancer (odds ratio 2.04) (6). In addition, the authors show, for the first time, that endometriosis is associated with ovarian low-grade serous ovarian carcinomas, doubling its risk in women with endometriosis (6). However, there was no association between endometriosis and high-grade serous carcinomas or other subtypes of ovarian cancer in the study.
Deligdisch and Nezhat et al. reported a series of 76 cases of stage I ovarian carcinomas and documented that non-serous carcinomas (54/76) were presented due to symptoms typically associated with endometriosis, including pelvic pain or vaginal bleeding associated with hyperestrogenism and endometrial pathology (4). Interestingly they also found that most high-grade serous carcinomas were found during evaluation of women with a history of breast cancer, or in women with BRCA mutation undergoing prophylactic salpingo-oophorectomy.
These and similar observations support the emerging dual model of epithelial ovarian carcinogenesis. According to this model, Type I ovarian carcinomas (low-grade serous, endometrioid, and clear cell carcinoma) are often associated with endometriosis. Type 2 carcinomas (high-grade serous) associated with TP53 mutations that are more aggressive and their origin is now thought to be fimbriated ends of fallopian tubal epithelium (5).
Taken together these findings will have considerable clinical implications and may affect the ways we think about strategies for ovarian cancer screening and prevention. In particular, the emerging knowledge of the link between ovarian cancer and endometriosis gives us an unprecedented opportunity to develop comprehensive screening plans to aid in the early detection and prevention of specific types of ovarian cancer in women with endometriosis.
While it is well known that most women with endometriosis do not develop ovarian cancer, women and their physicians should always discuss new findings, carefully document and discuss any new symptoms, and formulate plans for regular evaluation and treatment.
Endometriosis and Cancer Q & A
Similar to the way gynecological cancer patients are managed, Dr. Nezhat believes every endometriosis patient must be followed by a specialist in endometriosis, preferably a minimally invasive surgeon, for possible endometriosis recurrence and possible malignant transformation of endometriosis.
There are common characteristics between endometriosis and epithelial ovarian cancer:
- Metastatic (spreading from the initial site to another location) – local and distant
- Increased cell proliferation
- Invades and damages tissue
However, endometriosis does not cause catabolic or metabolic disturbances.
Epidemiological, histological, and molecular studies suggest a link between endometriosis and certain ovarian cancers, particularly the histological subgroups: endometrioid, clear cell, and low-grade serous ovarian carcinoma.
There is now an unprecedented opportunity to develop a comprehensive plan for women with endometriosis for early detection and prevention of specific types of ovarian cancers.
References:
- Levanon K, Crum C, Drapkin R. New insights into the pathogenesis of serous ovarian cancer and its clinical impact. J Clin Oncol. 2008 Nov 10;26(32):5284-93.
- Nezhat F, Datta MS, Hanson V, Pejovic T, Nezhat C, Nezhat C. The relationship of endometriosis and ovarian malignancy: a review. Fertil Steril. 2008 Nov;90(5):1559-70.
- Sampson JA. Endometrial carcinoma of the ovary arising in endometrial tissue in that organ. Arch Surg. 1925;10:1-72.
- Munksgaard PS, Blaakaer J. The association between endometriosis and ovarian cancer: a review of histological, genetic and molecular alterations. Gynecol Oncol. 2012 Jan;124(1):164-9.
- Deligdisch L, Pénault-Llorca F, Schlosshauer P, Altchek A, Peiretti M, Nezhat F. Stage I ovarian carcinoma: different clinical pathologic patterns. Fertil Steril. 2007 Oct;88(4):906-10.
- Pearce CL, Templeman C, Rossing MA, et al. on behalf of the Ovarian Cancer Association Consortium. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol. 2012 Apr;13(4):385-94.
Highlighted Publications:
- Nezhat FR, Apostol R, Nezhat C, Pejovic T. New insights in the pathophysiology of ovarian cancer and implications for screening and prevention. Am J Obstet Gynecol. 2015 Sep;213(3):262-7.
- Nezhat F, Apostol R, Mahmoud M, el Daouk M. Malignant transformation of endometriosis and its clinical significance. Fertil Steril. 2014 Aug;102(2):342-4.
- Nezhat FR, Pejovic T, Reis FM, Guo SW. The link between endometriosis and ovarian cancer: clinical implications. Int J Gynecol Cancer. 2014 May;24(4):623-8.
- Nezhat F, Datta MS, Hanson V, Pejovic T, Nezhat C, Nezhat C. The relationship of endometriosis and ovarian malignancy: a review. Fertil Steril. 2008 Nov;90(5):1559-70.
- Nezhat F, Cohen C, Rahaman J, Gretz H, Cole P, Kalir T. Comparative immunohistochemical studies of bcl-2 and p53 proteins in benign and malignant ovarian endometriotic cysts. Cancer. 2002 Jun 1;94(11):2935-40.
A listing of over 226 of Dr. Nezhat’s research articles can be found at the PubMed search engine, which pulls references and abstracts from the U.S. National Library of Medicine (NLM) database maintained at the National Institutes of Health (NIH).